A day at the NICU of Brigham and Women's Hospital. DtM Director of Product Development, Elizabeth Johansen, asks Dr. Steve Ringer and Respiratory Therapist Janet Rowell to try Pelican.
Yesterday was a great day for Design that Matter’s Pelican Pulse Oximeter project. Dr. Steven Ringer arranged for us to interview dozens of healthcare providers during an all-day visit at the Neonatal Intensive Care Unit of Brigham and Women’s hospital. During the day, we learned three very interesting things:
- moving parts and cables are the first to fail
- make it easy to wipe down
- a respiratory rate timer could be a great addition
Respiratory Therapist David Beadles tells DtM about common equipment failures at Brigham and Women’s Hospital.
Our host for the day was Respiratory Therapist David Beadles. We spoke about one of the inspirations for our project: the adult fingertip pulse oximeters you can buy over-the-counter at CVS. He mentioned, “Springs are always the first thing to fail on those probes. Whenever you have moving parts, you have failure.” Then he took us to see a $2500 sensor cable from a transcutaneous newborn monitor that had worn out and frayed over time. How might we create a device that is portable, but won’t get lost or stolen, without using cables to tie it onto something?
Nurse Karen Riedel tries wiping down the student prototype, and then the shoe prototype.
We asked Nurse Karen Riedel how she would clean a pulse oximeter between uses. She promptly grabbed the nearby jar of cleaning wipes, put on her latex gloves, and wiped down each prototype. Overall the process went smoothly for all of the prototypes. In the process, Karen noted some difficult-to-clean crevasses on the student prototype near the sensor. Opening the shoe prototype, Karen said, “Oooh magnets! If it comes apart it is much easier to clean. A hard material is best for wiping down.” However, would the top and bottom of the shoe get separated and lost?
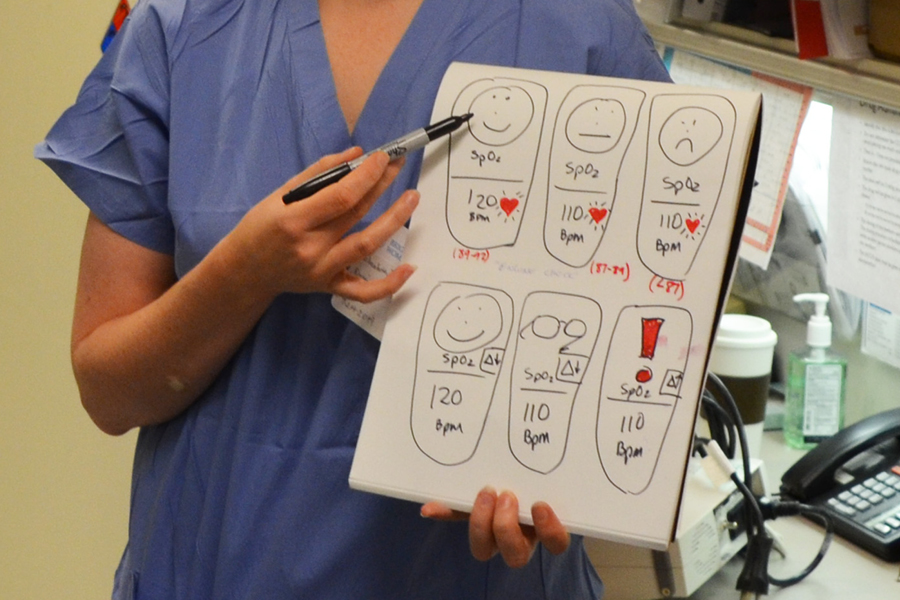
Respiratory Therapists Janet Rowell and Jill Robinson try the student prototype and dream about adding a timer to help them count newborn breath rate.
One of the biggest surprises of the day was learning how respiratory therapists at Brigham and Women's diagnose pneumonia. In addition to measuring oxygen level in the blood, therapists must measure how many breaths the newborn takes per minute. Respiratory Therapists Jill Robinson and Janet Rowell said the standard for measuring breath rate, even at this world-class hospital, is to look at the clock on the wall, then look at the newborn’s chest, and hope you look up at the clock again after 15-20 seconds, then multiply your reading to get breaths per minute.
Janet said, “Adding a stopwatch to your pulse oximeter would be great to help us count respiratory rate. Then you wouldn’t have to look away to see the clock on the wall.” Jill asked, “Could you add a function that keeps giving me a 15 second countdown over and over so I can count respiratory rate at any time? That would be very helpful for us!” If we add a timer to the device, it could better serve developing countries who follow the World Health Organization IMCI protocol which specifies counting breath rate. It was amazing to discover that the staff at the most resource-rich hospital could also benefit from a timer to help them count breath rates when diagnosing pneumonia and respiratory distress.
All in all it was a great day that gave us a great deal of new information and insights. We look forward to returning to the DtM studio to create a new round of prototypes to test next!
Click here to learn more about DtM's work with Brigham and Women's Hospital.